diabetes insipidus
- related: Endocrine
Diagnosis
- If urine output < 300cc/hr x3 hours, then get DI labs
- one dose dex won't interfere cortisol level
- random cortisol: 3-18 normal range
- use prednisone for secondary DI as no aldosterone needed. Does not need hydrocortisone
Causes
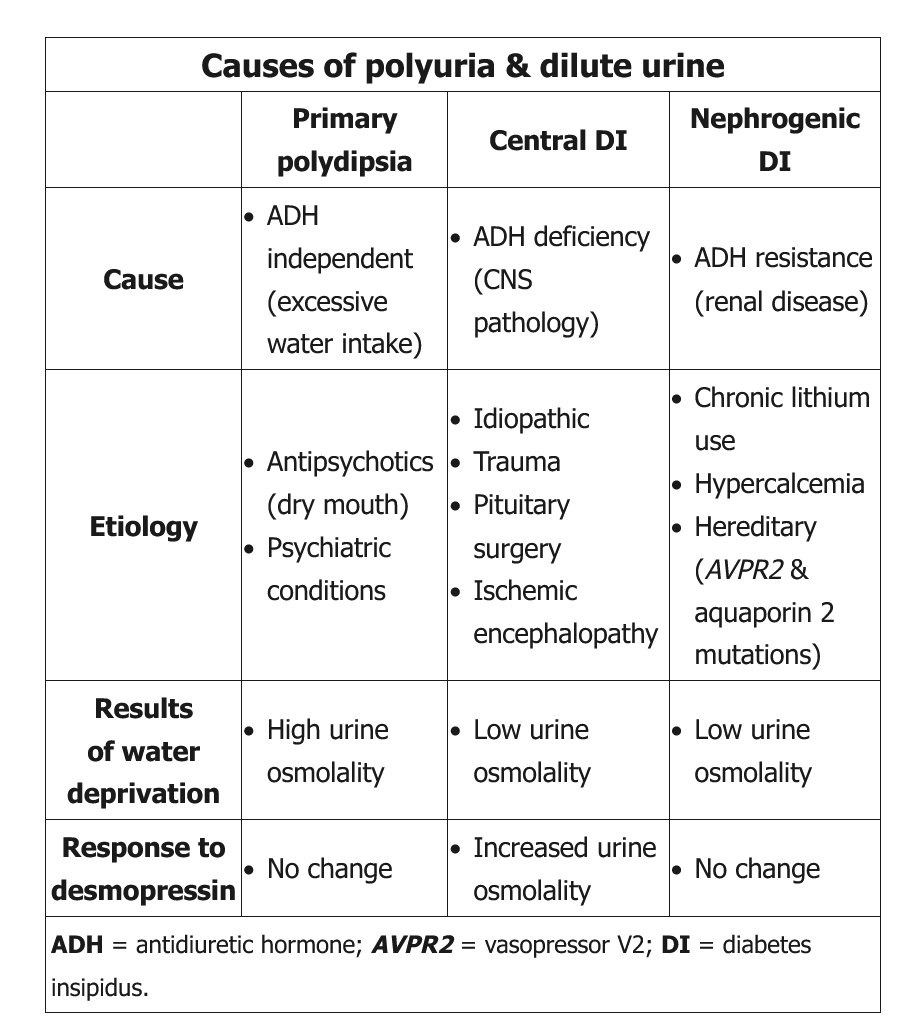
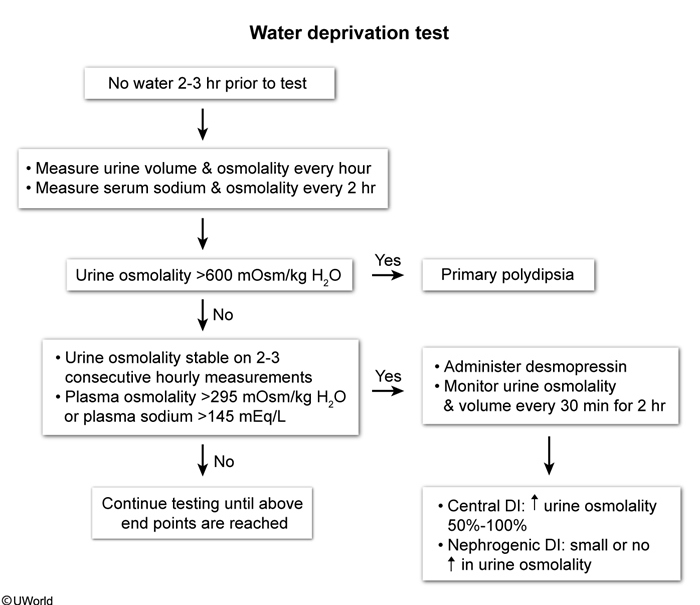
In addition to increasing the prednisone, the antidiuretic hormone (ADH) analogue desmopressin acetate is the most appropriate treatment. This patient most likely has central nervous system sarcoidosis and central diabetes insipidus (DI). Nearly half of hypothalamic-pituitary sarcoidosis cases occur in the course of previously treated sarcoidosis. Central DI results from inadequate release of ADH from the posterior pituitary gland. In the presence of ADH, aquaporin water channels are inserted in the collecting tubules and allow water to be reabsorbed. In the absence of ADH, excessive water is excreted by the kidneys. Frank hypernatremia is unusual because patients develop extreme thirst and polydipsia, and with free access to water, can maintain serum sodium in the high normal range. When patients do not drink enough to replace the water lost in the urine, due to poor or absent thirst drive or lack of free access to water, they develop hypernatremia. DI is diagnosed with simultaneous laboratory evidence of inability to concentrate urine (urine osmolality <300 mOsm/kg H2O) in the face of elevated serum sodium and osmolality. If necessary, a water deprivation test can confirm the diagnosis. A response to exogenous ADH would support a diagnosis of central DI, whereas a lack of response is seen in nephrogenic DI.
Central Diabetes Insipidus
Inability of the posterior pituitary gland to produce adequate antidiuretic hormone (ADH) results in central diabetes insipidus (DI). Absent antidiuretic hormone (ADH) (complete DI) and reduced ADH (partial DI) prevent the reabsorption of water in the kidneys resulting in polyuria and polydipsia. Although significant hypernatremia is rare in patients with an intact thirst mechanism and free access to water, it can be severe if patients cannot drink to thirst.
An inappropriately low urine osmolality in the setting of an elevated serum osmolality and hypernatremia in a patient with polyuria (>50 mL/kg/24 hours in the absence of glucosuria) is diagnostic of DI. A water deprivation test can be performed when the diagnosis is uncertain (see Table 18).
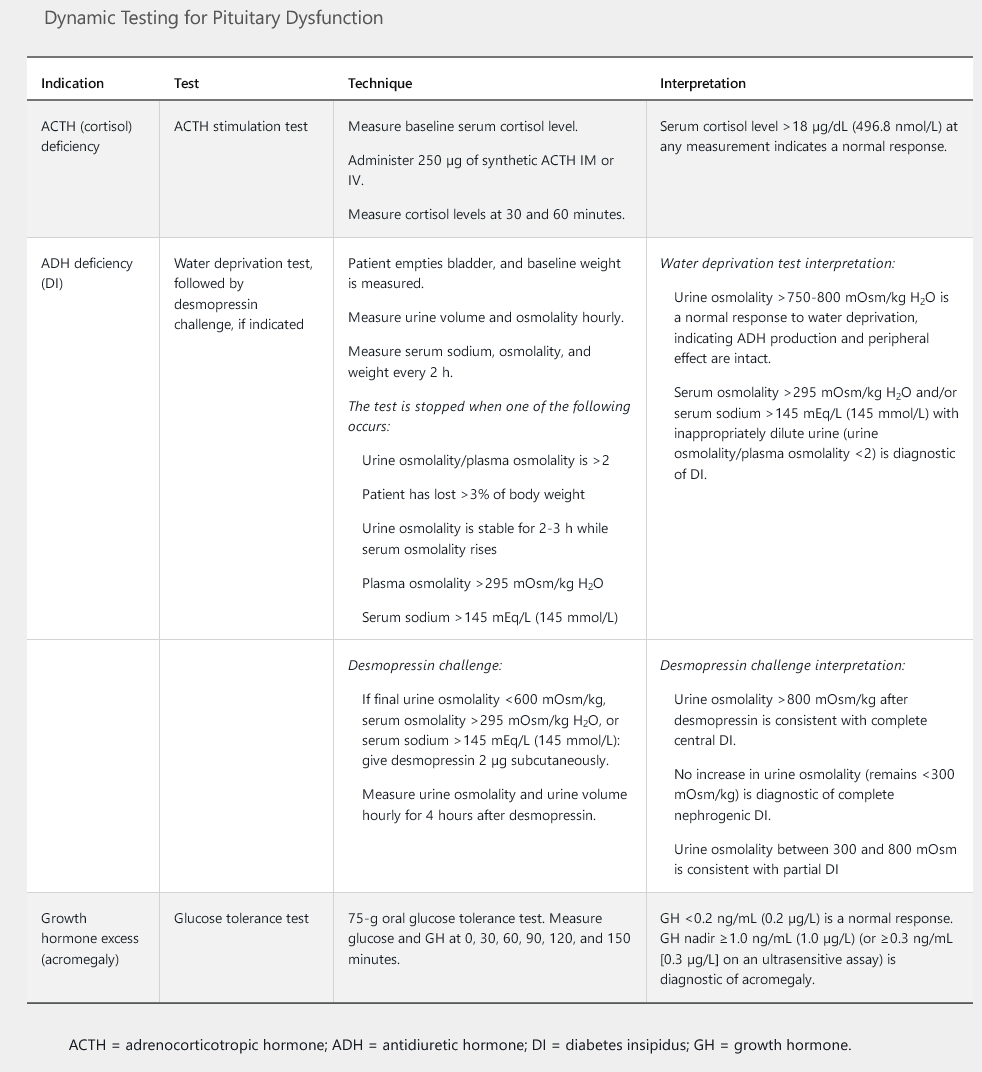
DI is treated with desmopressin (DDAVP) administered intranasally, orally, or subcutaneously. Bioavailability of oral DDAVP is much lower and doses are considerably higher than with intranasal and subcutaneous routes. Despite this, oral preparations may be preferred in certain circumstances as intranasal absorption of DDAVP may be altered by changes in nasal mucosa. Doses are usually administered once nightly to prevent nocturia and ensure uninterrupted sleep, or twice daily if symptoms interfere with daily function. Caution should be taken to avoid overreplacement as this can result in hyponatremia, water intoxication, and volume overload.
Nephrogenic